Chronic Kidney disease (CKD), also called chronic renal failure, is the irreversible loss of renal function due to replacement of functional nephrons with fibrous scar tissue. Kidneys filter wastes and excess fluids from blood, which are then excreted in urine. When chronic renal failure reaches an advanced stage, dangerous levels of fluid, electrolytes and wastes can build up in body.
In early stage of chronic renal failure, become clinically apparent as renal insufficiency, evidenced by azotemia and possibly polyurea and nocturia resulting from impaired tubular transport and concentration of urine. This Disease may not become apparent until kidney function is significantly impaired. Chronic renal failure can progress to end-stage kidney failure, which is fatal without artificial filtering (dialysis) or a kidney transplant.
Chronic renal failure represents progressive and irreversible destruction of kidney structures, leading to the accumulation of metabolic products, drugs and poisons, and
disorders of water, electrolyte, acid-base balance, and renal endocrine functions.
Related: Acute Renal Failure /Acute Kidney Failure
Chronic Renal / Kidney Failure Causes
This Disease occurs when a disease or condition impairs kidney function,
causing kidney damage to worsen over several months or years. Diseases and conditions that commonly cause include:
- Type 1 or type 2 diabetes,
- High blood pressure.
One of the complications resulting from diabetes or high blood pressure is the damage to the small blood vessels in the body. The blood vessels in the kidneys also become damaged, resulting in CKD. The most common cause of end-stage renal failure worldwide is IgA nephropathy (Inflammation in the kidney). Other common causes include:
- Recurring pyelonephritis (kidney infection).
- Polycystic kidney disease (multiple cysts in the kidneys), Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers.
- Autoimmune disorders such as systemic lupus erythematosus.
- Hardening of the arteries, which can damage blood vessels in the kidney.
- Urinary tract blockages and reflux, due to frequent infections, stones, or an anatomical abnormality that happened at birth.
- Excessive use of medications that are excreted through the kidneys.
- Vesicoureteral reflux, a condition that causes urine to back up into kidneys.
Pathophysiology Of Chronic Renal / Kidney Failure
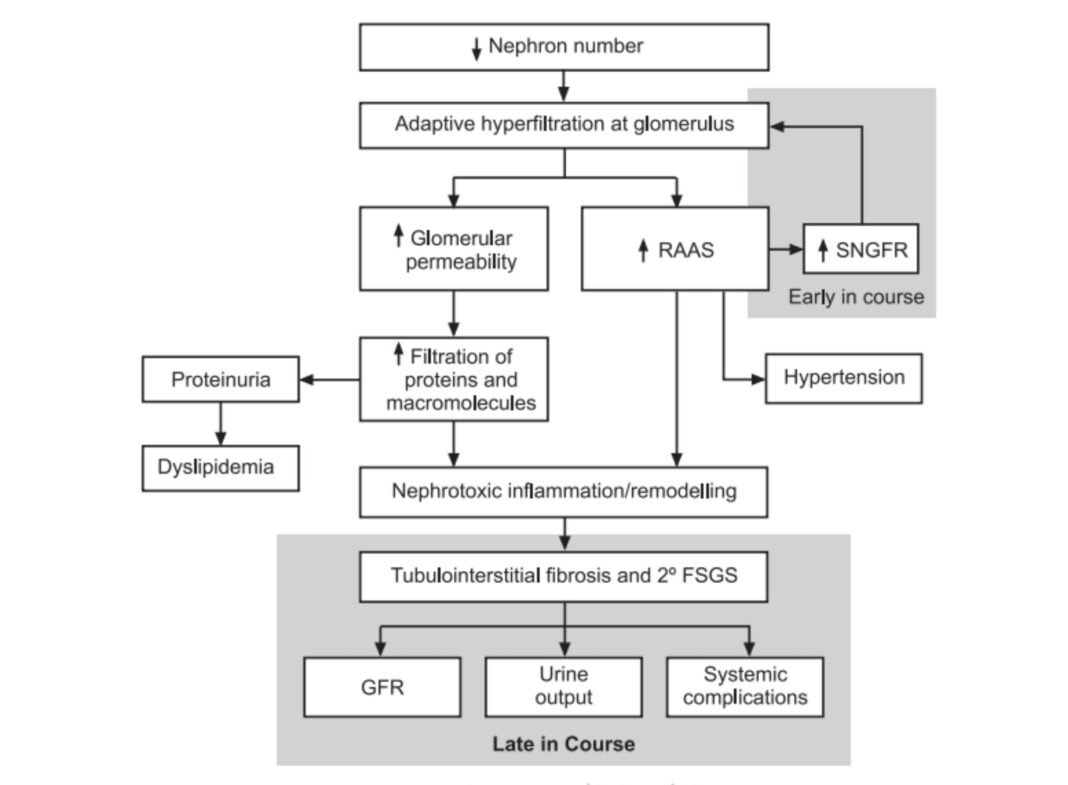
A normal kidney contains approximately 1 million nephrons, each of which contributes to the total glomerular filtration rate (GFR). In the face of renal injury (regardless of the etiology), the kidney has an innate ability to maintain GFR, despite progressive destruction of nephrons, as the remaining healthy nephrons manifest hyperfiltration and compensatory hypertrophy. This nephron adaptability allows for continued normal clearance of plasma solutes. Plasma levels of substances such as urea and creatinine start to show measurable increase only after total GFR has decreased to 50%.
The plasma creatinine value will approximately double with a 50% reduction in GFR. For example, a rise in plasma creatinine from a baseline value of 0.6 mg/dL to 1.2 mg/dL in a patient, although still within the adult reference range, actually represents a loss of 50% of functioning nephron mass. The increased glomerular capillary pressure may damage the capillaries, leading initially to secondary focal and segmental glomerulosclerosis (FSGS) and eventually to global glomerulosclerosis
Note : Refer The Diagram Above For Better Understanding!
Read Feeds
Acute Kidney Failure/Renal Diagnosis| Symptoms| Treatments and Drugs
Renal System.| What Is Renal System? | Kidney & Urinary System