Mechanism of inflammation pathophysiology | Acute Inflammation | What is acute inflammation with examples
Acute inflammation is of short duration and represents the early body reaction and is usually followed by healing.
examples :
- • Acute bronchitis
- • Sore throat from a cold or flu
- • A scratch/cut on the skin
- • Acute appendicitis
- • Acute dermatitis
The changes in acute inflammation can be conveniently described under the following two events and also categorized in the form of 2 events the are as follows.
- 1)Vascular Events
- a. Haemodynamic changes.
- b. Altered vascular permeability
- 2) Cellular Events
- a. Exudation of leukocytes
- b. Phagocytosis.
-
I) Vascular Events:
Alteration in the microvasculature (arterioles, capillaries and venules) is the earliest response to tissue injury. These alterations include hemodynamic changes and changes in vascular permeability.
-
a. Haemodynamic changes:
The earliest features of inflammatory response result from change in the vascular flow and caliber of small blood vessels in the injured tissue. The sequence of these changes is as under.
- Irrespective of the injury, immediate vascular response is the transient vasoconstriction of arterioles. With mild form of injury, the blood flow may be re established in 3-5 seconds. While with more severe injury, the vasoconstriction may last for about 5 min.
- Next follows persistent progressive vasodilatation which involves mainly the arterioles and lesser extents to venules and capillaries. This change is obvious within half an hour of injury. Vasodilatation results in increased blood volume in microvascular bed of the area, which is responsible for redness and warmth at the site of acute inflammation.
- Progressive vasodilatation in turn may elevate the local hydrostatic pressure resulting in transudation of fluid into the extracellular space. This is responsible for swelling at the local site of acute inflammation.
- Slowing or stasis is attributed to increased permeability of microvasculature that results in increased concentration of red cells and thus raised blood viscosity.
- Slowing or stasis is followed by leukocytes margination or peripheral orientation of leukocytes (mainly neutrophils) along the vascular endothelium. The leucocytes stick to the vascular endothelium briefly, and then move and migrate through the gaps between the endothelial cells into the extravascular space known as emigration.
The features of haemodynamic changes in inflammation are best demonstrated by
the Lewis experiment. Lewis induced the changes in the skin of inner aspect of
forearm by firm stroking with a blunt point. The reaction so elicited is known as triple
response or red line response consisting of the following:
- (i) Red line appears within a few
seconds following stroking and is
due to local vasodilation of
capillaries and venules. - (ii) Flares are the bright reddish
appearance or flush surrounding the
red line and results from
vasodilation of the adjacent
arterioles. - (iii) Wheal is the swelling or oedema of
the surrounding skin occurring due
to transudation of fluid into the
extravascular space.
-
b. Altered vascular permeability:
In acute inflammation, normally non permeable endothelial layer of microvasculature becomes leaky. This is explained by one or more of the following mechanisms.
- Contraction of endothelial cells: This is the most common mechanism of increased leakiness that affects venules exclusively, while capillaries and arterioles remain unaffected .The endothelial cells develop temporary gaps between them due to their contraction resulting in vascular leakiness. It is mediated by the release of histamine, bradykinin, and
other chemical mediators. The response begins immediately after injury, is usually reversible and is for short duration (15-30 minutes). - Retraction of endothelial cells: In this mechanism, there is structural reorganization of the cytoskeleton of endothelia cells that causes reversible retraction at the intercellular junctions. This change affects the venules and is mediated by cytokines such as Interleukin-1 (IL-1) and tumor necrosis factor α (TNF-α). The onset of response takes 4-6 hours after injury and lasts for 2-4 hours or more.
- Direct injury to endothelial cells: Direct injury to the endothelium causes cell necrosis and appearance of physical gaps at the sites of detached endothelial cells. Process of thrombosis is initiated at the site of damaged endothelial cells. The change affects all levels of microvasculature. The increased permeability may either appear immediately after injury and lasts for several hours or days (immediate sustained leakage) or may occur after a delay of 2-12 hours and last for hours to days (delayed prolonged leakage).
- Endothelial injury mediated by leukocytes: Adherence of leukocytes to the endothelium at the site of inflammation may results in activation of leukocytes. The activated leukocytes release proteolytic enzymes and toxic oxygen species which may cause endothelial injury and increased vascular leakiness. This form of increased vascular leakiness affects only venules is a late response.
- Other Mechanism: In addition, the newly formed capillaries during the process of repair are excessively leaky.
-
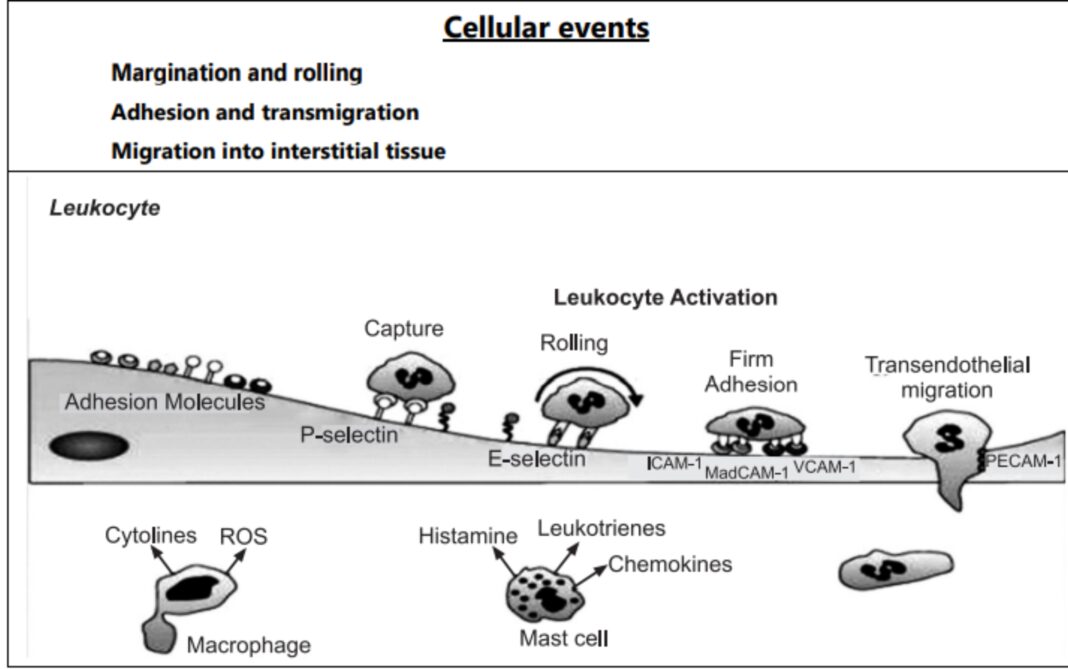
II) Cellular Events:
-
a. Exudation of leukocytes:
The escape of leukocytes from the lumen of microvasculature to the interstitial tissue is the most important feature of inflammatory
response. In acute inflammation, polymorpholonuclear neutrophils comprise
the first line of body defense, followed later by monocytes and macrophages.
The changes leading to migration of leukocytes are as follows:
- Changes in the formed elements of blood: In the early stage of inflammation
the rate of flow of blood increases due to vasodilation. But subsequently there is
slowing or stasis of blood stream. With stasis, changes in the normal axial flow of
blood in the microcirculation takes place. The normal axial flow consists of central
stream of cell comprised by leukocytes and RBC and peripheral cell free layer of plasma
close to vessel wall. Due to slowing and stasis, the central stream of cells widens and
peripheral plasma zone becomes narrower because of loss of plasma by exudation. This
phenomenon is known as ‘margination’. As a result of redistribution, the neutrophils of
the central column come close to the vessel wall, this is known as ‘pavementing’. - Rolling and Adhesion: Peripherally marginated and pavemented neutrophils slowly roll over the endothelial cell lining of the vessel wall (Rolling phase). Neutrophils first roll among the surface of the endothelium in a process mediated by selectins, adhesion molecules that are expressed by endothelial cells and that bind reversibly to sites on the leukocyte membrane. Later, neutrophils become firmly adherent to the endothelium by binding of leukocyte adhesion molecules (Selectins, Integrins, Intercellular adhesion molecules-1, vascular cell adhesion molecule-1, platelet endothelial cell adhesion molecule-1 etc.) This is followed by the transient bond between leukocytes and endothelial cells becoming firmer. (Adhesion phase). The following adhesion molecules bring about rolling and adhesion phases
- Transmigration: After sticking of neutrophils to endothelium, the former move along the endothelial cell is found where the neutrophils throw out cytoplasmic pseudopods. Subsequently the neutrophils are lodged between the endothelial cells and cross the basement membrane by damaging it locally with secreted collagenase and escape out into the extravascular space. This is known as ‘transmigration’. The damaged basement membrane is repaired almost immediately, simultaneous to emigration of leukocytes, escape of RBC’s through the gaps between the endothelial cells. It is passive phenomenon, RBCs being forced out either by raised hydrostatic pressure or may escape through the endothelial defects left after emigration of leukocytes.
- Chemotaxis: The movement of leukocytes from the vessel lumen into a damaged area is called chemotaxis and is mediated by substance known as chemotactic factors that diffuse from the area of tissue damage. All granulocytes and monocytes respond to chemotactic factors and move along a concentration gradient. Chemo attractants can be exogenous or endogenous. Most exogenous chemotactic factors are bacterial or other microbial products. There are many endogenous chemotactic factors like fibrin, fibrinopeptides, bacterial components, IL-8, IL-5, histamine, monocyte chemotactic factors (MCP-1 & MCP-5). Chemotactic factors bind to receptors on the surface of leukocytes and activate secondary messenger systems. These messenger systems work by stimulating increased intracytoplasmic calcium. The calcium then interacts with the cytoskeleton resulting in active movement of the cell.
b) Phagocytosis:
It is defined as “the process of engulfment of solid particulate material by the cells”. There are two main types of phagocytic cells:
- Polymorphonuclear neutrophils (PMN’s) which appear early in acute inflammatory response also called as microphage.
- Circulating Monocytes and fixed tissue mononuclear phagocytes are called as macrophages. Neutrophils and macrophages on reaching the tissue space produce several proteolytic enzymes lysozyme, protease, collagenase, elastase, lipase, proteinase, gelatinase and acid hydrolases. These enzymes degrade collagen and extracellular matrix that will kill bacteria.
Related reads:
Mechanism of Hypoxia | Signs And Symptoms| Free Radical Induced Injury
MORPHOLOGY OF CELL INJURY | ADAPTIVE CHANGES | CELLULAR SWELLING
CELL INJURY | Mechanism of cell injury | Pathogenesis| Morphology
Positive Feedback Mechanism Vs Negative Feedback Mechanism| Adaptation | Homeostasis