Etiology of Hypertension
The exact causes of high blood pressure are not known, but several factors and conditions may play a role in its development, including:
- Smoking
- Being overweight or obese
- Lack of physical activity
- Too much salt in the diet
- Too much alcohol consumption
- Stress
- People with family members who
have high blood pressure - Chronic renal failure
- Adrenal and thyroid disorders
Many people with kidney disorders have secondary hypertension. The kidneys
regulate the balance of salt and water in the body if the kidneys cannot rid the body of
excess salt and water, blood pressure goes up. Kidney infections, a narrowing of the
arteries that carry blood to the kidneys, called renal artery stenosis and other kidney disorders can disturb the salt and water balance. Cushing’s syndrome and tumors of the pituitary and adrenal glands often increase levels of the adrenal gland hormones like
cortisol, adrenaline and aldosterone, which can cause hypertension. Certain medications, such as birth control pills, cold remedies, decongestants, over-the-counter pain relievers and some prescription drugs, illegal drugs, such as cocaine and amphetamines or chronic
alcohol use, obstructive sleep apnea and pregnancy may lead to hypertension.
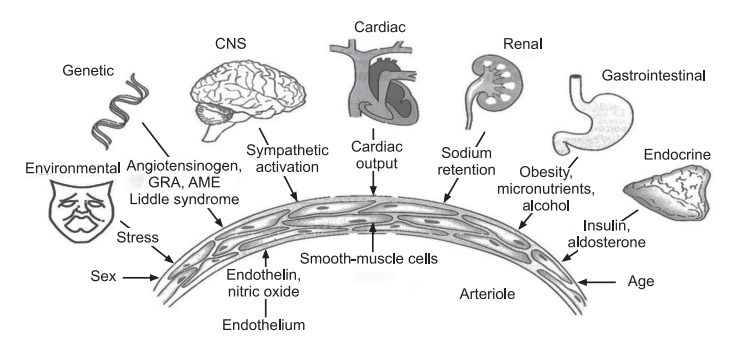
Pathophysiology of Hypertension
Hypertension causes three major circulatory abnormalities: increased arteriolar resistance, increased large artery stiffness, and early or premature reflection
of arterial pulse waves. Increased resistance and vessel stiffness in younger hypertensive patients result from structural changes, including thinning and fracturing of elastin, increased collagen deposition, and increased wall thickness. These changes manifest primarily as a greater rise in systolic pressure greater than diastolic pressure. In elderly, an increased arterial stiffness is the greater factor and may contribute to isolated systolic hypertension, in which systolic pressure is elevated but diastolic pressure is normal or low. Patients with isolated systolic hypertension are at substantially increased risk for stroke,
coronary heart disease, and congestive heart failure. Pulse wave reflection referes to the
backward rebound of some of the cardiac output as it encounters the resistance of the
arteries. When arteries are normally complaint, this reflected flow occurs during
diastole and assists with filling of the coronary arteries. In hypertension, however,
reflection occurs prematurely, during systole, contributing to vascular overload in
the aortic arch and in the coronary carotid and renal arteries.
Secondary hypertension accounts for approximately 5-10% of all cases of hypertension, with the remaining being primary hypertension. Secondary hypertension has an
identifiable cause whereas primary hypertension has no known cause (i.e.
idiopathic). There are many known conditions that can cause secondary hypertension. Regardless of the cause, arterial pressure becomes elevated either due to an increase
in cardiac output, an increase in systemic vascular resistance, or both. When cardiac
output is elevated, it is generally due to either increased neurohumoral activation of
the heart or increased blood. Increased systemic vascular resistance is most
commonly caused, at least initially, by increased sympathetic activation or by the
effects of circulating vasoconstrictors (e.g., angiotensin II). Anatomic considerations, such as narrowing of the aorta (e.g., coarctation) or chronic changes in vascular structure (e.g., vascular hypertropy) can also cause or contribute to increased systemic vascular resistance. Renal artery disease can cause because of narrowing of the vessel lumen (stenosis). The reduced lumen diameter decreases the pressure at the afferent arteriole in the kidney and reduces renal perfusion. This stimulates renin release by the kidney, which increases circulating angiotensin II and aldosterone. These hormones increase blood volume by enhancing renal reabsorption of sodium and water. Increased angiotensin II also causes systemic vasoconstriction and enhances sympathetic activity. Chronic elevation of angiotensin II promotes cardiac and vascular hypertrophy. The net effect of these renal
mechanisms is an increase in blood volume that augments cardiac output. Therefore, hypertension caused by renal artery stenosis results from both an increase in systemic vascular resistance and an increase in cardiac output.
- Chronic renal failure: A number of pathologic processes (e.g., diabetic nephropathy, glomerulonephritis) can damage nephrons in the kidney. When this occurs, the kidney cannot excrete normal amount of sodium which leads to sodium and water retention, increased blood volume, and increased cardiac output by the Frank-Starling mechanism. Renal disease may also result in increased release of renin leading to a renin dependent form of hypertension. The elevation in arterial pressure secondary to renal disease can be viewed as an attempt by the kidney to increase renal perfusion and restore glomerular filtration.
- Primary hyperaldosteronism: Increased secretion of aldosterone generally results from adrenal adenoma or adrenal hyperplasia. Increased circulating aldosterone causes renal retention of sodium and water, so blood volume and arterial pressure increases. Plasma renin levels are generally decreased as the body attempts to suppress the renin-angiotensin system; there is also hypokalemia associated with the high levels of aldosterone.
- Stress: Emotional stress leads to activation of the sympathetic nervous system, which causes increased release of norepinephrine from sympathetic nerves in the heart and blood vessels, leading to increased cardiac output and increased systemic vascular resistance. Furthermore, the adrenal medulla secretes more catecholamines (epinephrine and norepinephrine). Activation of the sympathetic nervous system increases circulating angiotensin II, aldosterone, and vasopressin, which can increase systemic vascular resistance. Prolonged elevation of angiotensin II and catecholamines can lead to cardiac and vascular hypertrophy, both of which can contribute to a sustained increase in blood
pressure.
- Sleep Apnea: Sleep apnea is a disorder in which people repeatedly stop breathing
for short periods of time (10-30 seconds) during their sleep. This condition is often
associated with obesity, although it can have other causes such as airway obstruction or
disorders of the central nervous system. These individuals have a higher incidence of
hypertension. The mechanism of hypertension may be related to sympathetic activation and hormonal changes associated with repeated periods of apnea-induced hypoxia and hypercapnea, and from stress associated with the loss of sleep.
- Pheochromocytoma: Catecholamine secreting tumors in the adrenal medulla can lead to very high levels of circulating catecholamines (both epinephrine and norepinephrine). This leads to α-adrenoceptor mediated systemic vasoconstriction and β-adrenoceptor mediated cardiac stimulation, both of which contribute to significant elevations in arterial pressure. Despite the elevation in arterial pressure, tachycardia occurs because of the direct effects of the catecholamines on the heart and vasculature. Excessive β-adrenoceptor stimulation in the heart often leads to arrhythmias. The pheochromocytoma is diagnosed by measuring plasma or urine catecholamine levels and their metabolites (vanillylmandelic acid and metanephrine).
- Preeclampsia: This is a condition that sometimes develops during the third
trimester of pregnancy that causes hypertension, sometimes with fluid retension and priteinuria due to increased blood volume and tachycardia. The former increases cardiac output by the Frank Starling mechanism. Arch of the aorta: Obstruction of the
aorta at this point reduces distal arterial pressures and elevates arterial pressures in
the head and arms. The reduced systemic arterial pressure activates the renin angiotensin-aldosterone system, which leads to an increase in blood volume. This further increases arterial pressures in the upper body and may largely offset the reduction in lower body arterial pressures. This condition is readily diagnosed by comparing arterial pressures measured in the arms and legs. Normally, these pressures are very similar, but with coarctation, arterial pressures in the arms can be much greater than arterial pressures measured in the legs. Because this is a chronic condition, the baroreceptors are desensitized and upper body arterial pressures remain elevated because of the increased cardiac output to these parts of the body.
- Aortic coarctation: Coarctation (narrowing) of the aorta is a congenital defect that most commonly is found just distal to the left subclavian artery in the arch of aorta.
Epidemiology Of High blood pressure |Hypertension
As per the World Health Statistics 2012, of the estimated 57 million global deaths in
2008, 36 million (63%) were due to non communicable diseases (NCDs). The largest proportion of NCD deaths is caused by cardiovascular diseases (48%). In terms of
attributable deaths, raised blood pressure is one of the leading behavioral and
physiological risk factor to which 13% of global deaths are attributed. Hypertension is
reported to be the fourth contributor to premature death in developed countries and
the seventh in developing countries. Recent reports indicate that nearly 1 billion adults
(more than a quarter of the world’s population) had hypertension in 2000, and
this is predicted to increase to 1.56 billion by 2025. Earlier reports also suggest that the prevalence of hypertension is rapidly increasing in developing countries and is
one of the leading causes of death and disability.
Children: Most childhood hypertension, particularly in preadolescents, is secondary
to an underlying disorder. Apart from obesity, kidney disease is the most common
(60–70%) cause of hypertension in children. Adolescents usually have primary (essential)
hypertension, which accounts for 85–95% of cases
Related Reads:
Hypertension | Types of Hypertension(BP)^ | Nitric Oxide Pulmonary